The World’s Leading Eye Doctor Specializing in Corneal Scar Correction in Jacksonville
The worst insult from a pathology, disease, or dystrophy of the cornea or complication of any cornea-based surgery including LASIK, Contact lens infection, etc. is a corneal scar. Corneal scars can blind people. With over three decades of correcting corneal scars straight to vision, Dr. Gulani has seen practically every possible type of corneal scar and helped patients from all over the world.
Making Corneal Transplants Extinct: Gulani Corneoplastique®:
Dr. Gulani has been correcting blinding corneal scars of all kinds straight to vision without transplants with his proprietary Laser Corneoplastique® techniques honed over three decades. Using a wide range of techniques and technology, KLEARTM , many patients have been brought to vision within minutes when they were relegated by their surgeons to invasive corneal transplant options only.
Numerous patients from all over the world in need of corneal scar correction of varied causes like LASIK and PRK complications, contact lens infections, dystrophy, etc. have been corrected with Dr. Gulani’s cutting-edge, least interventional, no-blade, no-cut procedures in single or staged combinations keeping corneal transplant as a last resort.
Symptoms:
Having seen a wide variety of corneal scar patients from all over the world, the most common symptoms they have, despite their unique situations, include: blurred vision, halos around lights, starbursts, double or distorted vision, difficulty driving at night, and vision fatigue. Most patients travel to us desperate for help having been denied opportunities by their eye doctors and surgeons who have assumed their own inability or the patient’s lack of potential to see. Often, relegating patients to less than optimal options (like invasive corneal transplants or uncomfortable hard contact lenses) or telling patients to “live with it” or there is “nothing we can do”.
Corneal Scar Correction Treatments:
“A doctor’s inability should never become the patient’s disability,” says Dr. Gulani, who teaches worldwide to encourage every ophthalmologist (eye surgeon), optometrist, and all levels of eye care providers to fight for their patients’ vision. Though we cannot guarantee outcomes in such complex corneal scar cases, 1000’s of patients have shared their testimonials and stories (with no incentive) on our website with a desire to spread hope among fellow patients and possibly inspire their eye surgeons to perform.
Using Advanced Diagnostics during his personal consultation and years of clinical acumen, Dr. Gulani first determines what kind of corneal scars you have along with associated refractive errors (i.e. irregular astigmatism, myopia, hyperopia, presbyopia, etc.) and pathologies (i.e. Cataracts, Fuchs Dystrophy, etc.), and additional surgeries (i.e. LASIK, Cataract Surgeries, Cross-Linking, etc.), then based on his proprietary algorithm honed over three decades picks among the full spectrum of surgical and technological options (KLEARTM) to custom design a procedure and technology application to best correct your unique eyes and can even help patients with extreme situations which is innovative, staged, and combination techniques.
As a renowned corneal transplant surgeon himself, Dr. Gulani believes transplants should be the last option for corneal scar patients because not only are they an interventional surgery that involves donor tissue (that can be rejected), but also because it doesn’t lead to vision with freedom from contact lenses or glasses.
If for some reason you have already undergone cross-linking, a corneal transplant, cataract surgery, or wear contact lenses, you still don’t need to despair. Though this may decrease your chance of reaching a 20/20 outcome, Dr. Gulani has successfully corrected numerous such corneal scar patients from all over the world.
With a legendary track record of successful vision outcomes, Dr. Gulani continues to create and envision the future to pursue his passion to help people see.



Following a detailed personal consultation with the patient along with advanced diagnostic testing he classifies corneal scars as follows:
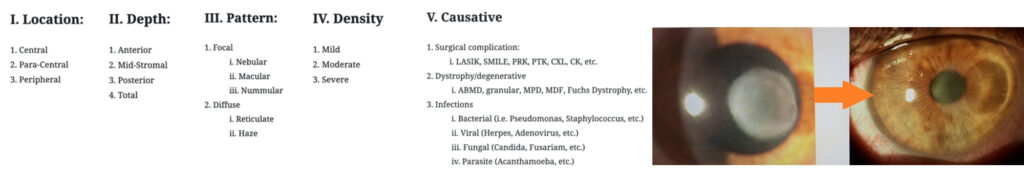
Armed with this detailed knowledge Dr. Gulani then determines to address as many of these as he humanly can. This can be done in a single or staged approach. Unleashing a uniquely designed surgical plan with cutting-edge technology and technique application Dr. Gulani has brought thousands of patients from all over the world to their best vision potential.
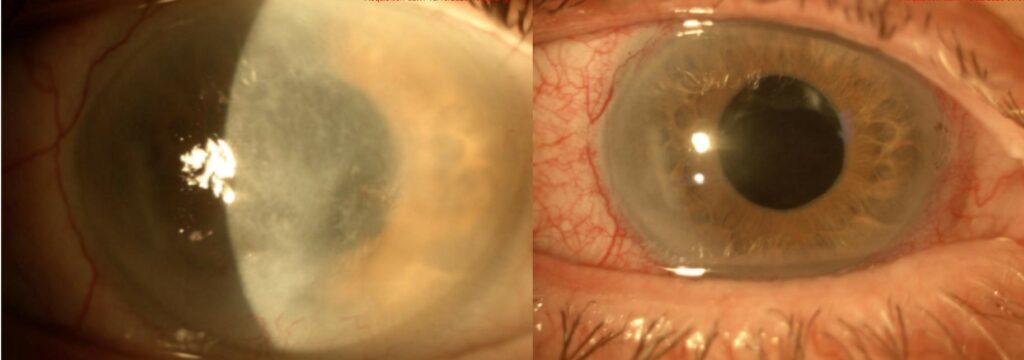
The traditional thinking for a corneal scar has always been to get rid of it and the tissue that contains it ie. Corneal transplant.
When looking at a corneal scar, our inherent mindset is : “There is the culprit. Let’s eradicate it.” Numerous diagnostic technologies are then deployed to “Understand the scar and its obviously criminal impact on Vision.”
Then—in their minds—many ophthalmologists go through an elegant and complicated thought process to determine whether to choose laser PTK (an optically incorrect surgery), diamond burr application (a barbaric procedure on an elegant visual organ), or a corneal transplant (a relatively interventional procedure that should be the last resort, very much like having to finally open the entire abdomen to get to the gall bladder) as the correct treatment for this corneal scar.
Let us assume also a mindset that thinking about performing a corneal graft (Penetrating keratoplasty: PKP) is akin to giving up, losing the battle, or not even venturing to design vision in our patient’s best interests. Unless there is a through-and-through corneal pathology/perforation from whatever cause (trauma, infection, surgical complications, degeneration, etc.), a penetrating corneal transplant should be the last resort of corneal rehabilitative techniques.
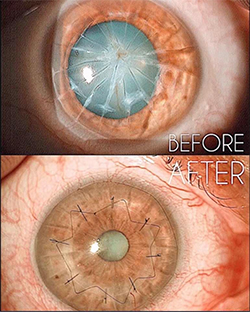
As I have said before, PKP can be compared to opening the entire abdomen as opposed to elegantly approaching individual structures with the least interventional attitude. It does not matter how you do the penetrating transplant, i.e., femtolaser, microkeratome, or even a kitchen knife; what matters is how you put it back together (since shape translates to refraction and refraction translates to vision) and hand stitching of the transplant leads to astigmatism and vision distortion, not to mention rejection issues including heightened possibility of glaucoma, cataracts and lifetime danger of the graft coming apart with trauma.
Using our 5S system, most corneas that are structurally abnormal, unstable, or compromised should undergo an elegant thought process using Corneoplastique® principles (brief, topical, aesthetically pleasing, visually promising) to rehabilitate that cornea with the least interventional approach for that patient and present it as a vision rehabilitative platform (VRP).
What I suggest instead is to look at the corneal scar and ask yourself, “How can I use this or modify this to help the patient see better with the least intervention” and “Is it necessary to remove this and at what cost?”
This is the paradigm shift in thinking and the future of molding corneal scars to our advantage (by whatever surgical means and combinations) to therewith improve refraction and hence the vision.
Anterior corneal scars affect vision directly by blocking the optical pathway, and indirectly, by altering the shape, and hence the refractive status. Using Corneoplastique® principles, we can use these very factors and reverse them to our advantage.
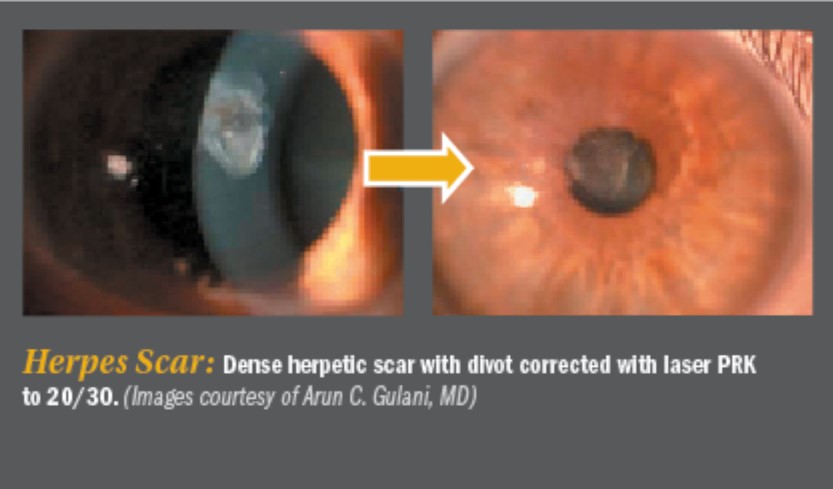
In the Gulani 5S algorithm, you can see the impact of the corneal scar on vision and determine the patterned approach of corneal rehabilitation and laser or direct laser, and straight reshaping to vision. The refraction is the mainstay of the corneal scar algorithm, where vision better than 20/30 suggests straight laser LaZrplastique®; while less than 20/40, following a hard contact lens trial, can determine staged laser in two stages or a scar peel, followed by myopic ablation.
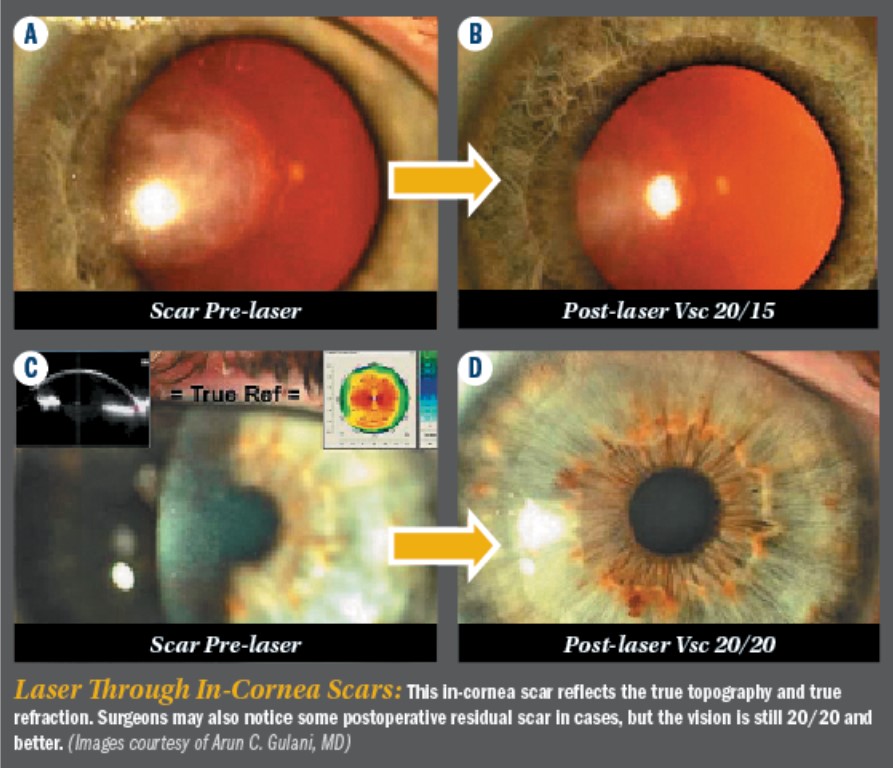
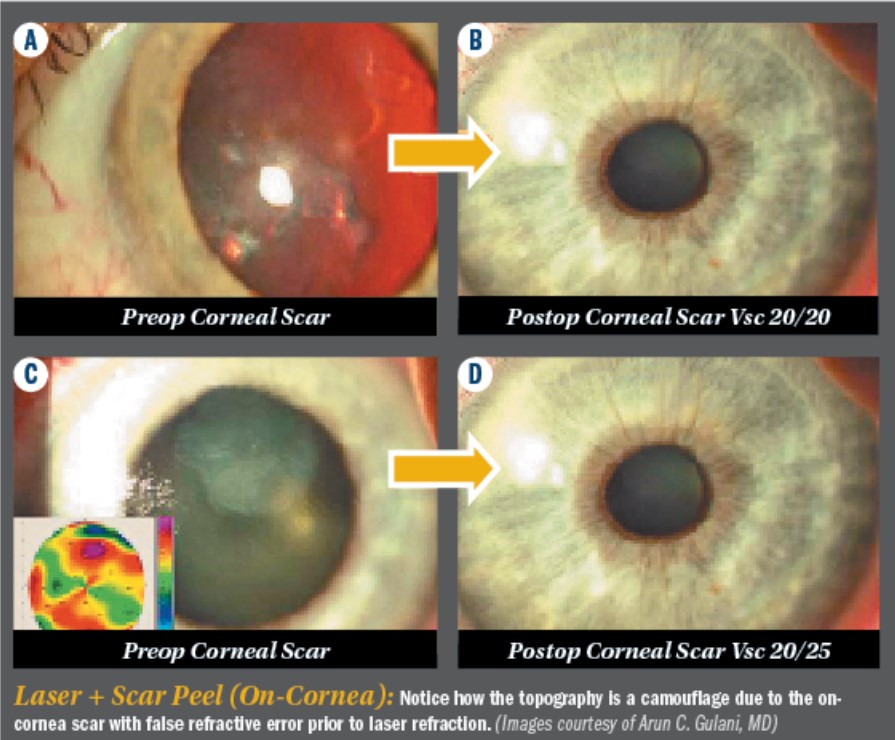
For the sake of simplicity, I have divided corneal scars into ‘on-cornea’ scars, which are above the Bowman’s membrane and lead to a camouflaged topography and misleading refractive error and “In-cornea’ scars, which actually become part of the cornea and are directly responsible for the topography, and have a direct correlate to the refractive error. Hence, these can be lasered through.
Instead of laser PTK, which chases the scar and distorts the shape (costing us in vision), why not reshape the cornea and take it straight to vision (in many cases, despite a residual scar)?
Understanding On-cornea and In-cornea scars
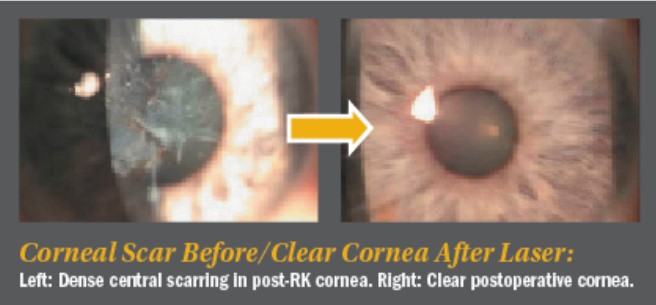
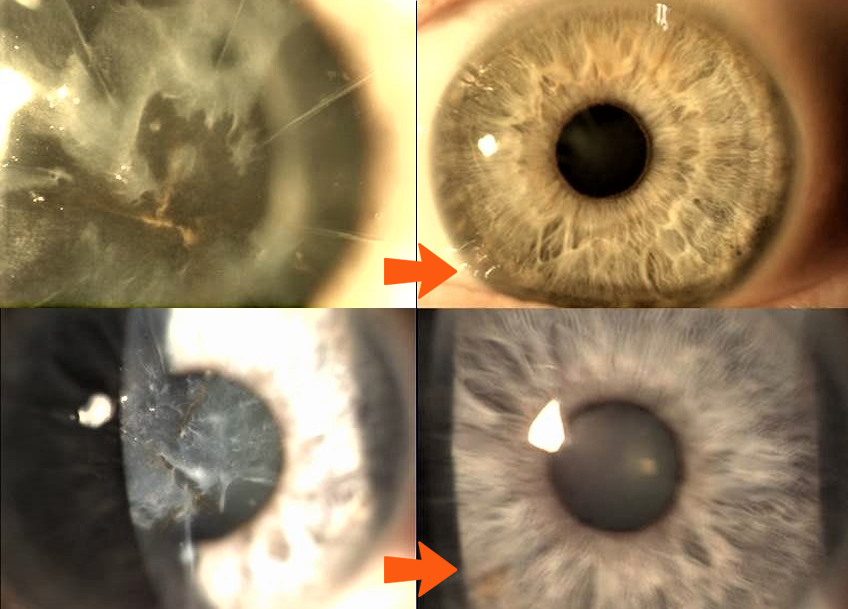
On-cornea scars can be peeled off right under the laser using the cornea as what I call a “resistance-guided platform” which is comprised of pulling on the scar, making sure you remove it completely, in one piece, using the rest of the cornea as your resistance platform. This is followed by Refractive LaZrplastique® (always with mitomycin C application)as single stage or Myopic LaZrplastique® to be followed by stage two for refractive LaZrplastique® to emmetropia.
Deeper on-cornea scars can also be peeled off using patience and a resistance-guided technique as well to gently peel them off of the rest of the cornea. Once again, try to maintain the entire piece as a single removal technique. Once it clears the visual axis, you can proceed with refractive laser LaZrplastique® ablation, followed again by the application of mitomycin C. This can result in complete central clarity, to an excellent outcome.
In-cornea scars can be Lasered directly in the ASA mode, shaping the cornea, and indirectly removing the scar, straight to a visual outcome. In cases of on-cornea scars, the scar can be gently peeled off, maintaining all the principles we discussed about using the corneal platform as a resistance guided technique in lifting the entire scar gently, in full completion, off the remaining cornea. This is followed by LaZrplastique® with mitomycin C and a bandage contact lens, to reach tremendous visual outcomes (Single or Two-Staged).

Lens Based Optical Manipulation to Prepare Corneal VRP:
Intra-ocular optical manipulation in the form of lens based (pseudophakic and phakic implants) techniques can be combined to aim for Myopic LaZrplastique® before or after as second stage (Endpoint always being Emmetropia with indirect goal of scar removal)
No matter how bad the scar looks, let us use our algorithm to insist on taking patients straight to vision, with the most elegance possible, maintaining the principles of Corneoplastique® surgery—topical, brief, aesthetically pleasing, and visually promising.
Refractive laser LaZrplastique®surgery—when practiced as an art—can not only address virgin eyes with all levels of ametropia, but also reverse and correct complex as well as complicated cases with corneal scars back to 20/20 vision. Refractive surgery truly then, can come to its own rescue!
When Corneal involvement is more that superficial and unstable:
Let us consider a cornea in which the structural instability stems from it being extremely thin and irregular, including deeper levels of scar involvement. Such cases can be elegantly built by imagining that the cornea consists of layers; hence, lamellar keratoplasty in the form of anterior sutureless, anterior sutured, deep anterior lamellar keratoplasty, or posterior lamellar techniques can be performed to rehabilitate the cornea (thus removing Scar and improving Site) and add donor tissue (plus improving Strength) for future laser reshaping (improving Shape. which equals to vision).
By the same token, corneas that are extensively thickened by surgeries such as epikeratophakia, can undergo removal of the epilenticle to restore the corneal anatomy and present it for final laser reshaping. Physiologically speaking, corneas thickened by Fuch’s dystrophy can be rehabilitated using DSAEK/DMEK surgeries to revitalize the cornea to its normal anatomy and thickness for future laser reshaping.
Of course, in cases that demand correction of through-and-through corneal anomalies—such as perforation, degeneration, etc.—a penetrating corneal transplant can be suggested as the last resort, and then again, in preparation for future laser reshaping after suture removal.
In our aggressive desire to be least interventional, we see this pattern of changing, adding, or removing specific corneal lamellae in a structurally focused fashion to restore normalcy in the anatomy and physiology of the cornea to present it as the most accessible part of the eye in reshaping it with the Excimer laser towards BVP (best vision potential) and emmetropia.
In cases of moderate anatomical abnormality with structural instability (i.e., keratoconus, keratoglobus, pellucid marginal degeneration, or LASIK ectasia), INTACS can be used in an intelligently-applied, asymmetric fashion using different ring combinations (i.e., 0.45 and 0.3), superficial and deep placement, single and paired rings, and incision placement manipulation.
The INTACS then act as braces in this unstable cornea, to first correct the progress of the abnormality, and second—in a case-specific, customized fashion—to visually focus the rehabilitated cornea and further present it for laser vision surgery to correct astigmatism, which is the most common error with keratoconus that removes the least amount of tissue with the Excimer laser.



Ocular surface pathologies such as advanced pterygium, recurrent pterygium, limbal lesions can be addressed with amniotic membrane reconstruction to clear the pathology on the cornea and rehabilitate the ocular surface to present the cornea for vision corrective surgery once again. Not only is it the need of the hour for such amniotic surface procedures to be cosmetically appealing, but also they should be visually propulsive in directing the next step of corneal reshaping or intraocular optical correction (ICL or premium lens implants) to BVP.
Having rehabilitated the cornea in many of these aforementioned forms, in single or combination processes, collagen cross-linking (CCx) can be used to permanize and stabilize the restored cornea prior to laser reshaping or after laser reshaping.
Intraocular optical manipulations using monofocal, toric, piggy-back, phakic lens implants can be used to emerge with myopic endpoints in preparation for future staged laser reshaping towards emmetropia and BVP. Myopic laser reshaping corrects the central cornea of the scar, increases the optical zone, smoothens the anterior surface, and also addresses ametropia- directly.
In summary, we see how the cornea can be prepared for laser vision surgery and repaired from laser vision surgery, or basically, any kind of kerato-refractive surgery coming to its own rescue. Using the above armamentarium of techniques and technologies, practically every eye deserves a chance towards planned emmetropia using least intervention and visually focused direct techniques, thus presenting the cornea as a vision rehabilitative platform for laser vision correction.