The World's Leading Pterygium Surgeon in Jacksonville
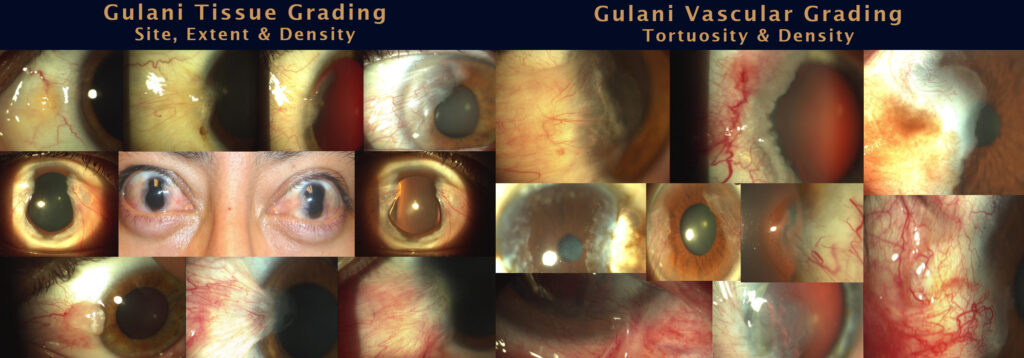
Pterygium (derived from the Greek word “pterygos” meaning wing) is a reddish triangular fibro-vascular lesion (bump) that usually occurs on the white of the eye. The worldwide prevalence of pterygium is around 10.2% with increased incidence in the tropics and equatorial zones with associated sun exposure and outdoor activities therein commonly also called “surfer’s eye”, “golfer’s eye”, etc. Presentations vary in various tissue distributions and vascular patterns from small atrophic lesions to large aggressive vision-compromising growths in advanced cases.

Symptoms:
Pterygium patients seek Dr. Gulani from all over the world with a desire to have a cosmetically appealing eye along with resolution of common symptoms like red, irritated eyes with associated dryness and even scarring which can impact vision adversely in advanced cases.
While teaching pterygium surgery globally, Dr. Gulani encourages eye surgeons to empathize with patients who complain about pterygium and genuinely understand their suffering which could range in severity from patients’ heightened self-consciousness about appearance, lowered self-esteem, even to the point of depression.
Primary pterygium is so designated in cases that have not had previous pterygium surgeries. Approaching each pterygium in a custom designed surgical fashion Dr. Gulani further classifies pterygiums into:
- Mild
- Medium
- Large
- Progressive
- Non-Progressive
- Fleshy
- Atrophic
- Unilateral
a. Medial: toward the nose
b. Lateral: towards outer part of the eye
c. Superior or Inferior: less common locations - Bi-temporal: on each side of the eye
- Circumferential
Diagnostics and Treatment:
In a detailed personal consultation with advanced technology, Dr. Gulani evaluates not only the pterygium and its anatomical and optical impact, but also associated dry eyes and visual status to then custom design his treatment and surgical plans to each patient to deliver the best outcome with the safest approach in that patient’s best interest.
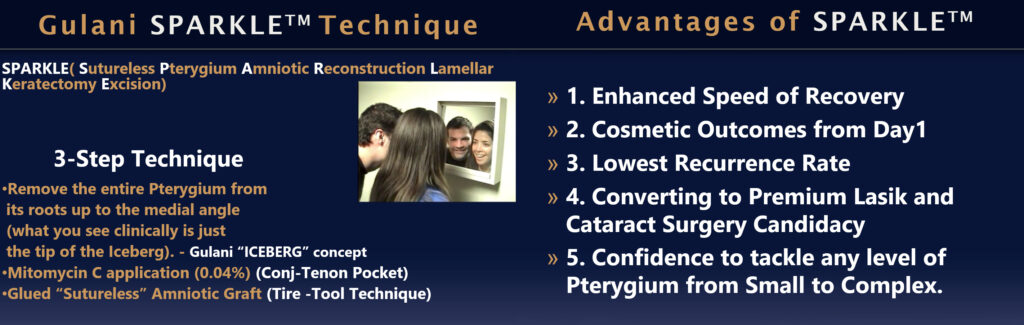
Dr. Gulani over three decades has honed his “No-Stitch” surgical technique; SPARKLE™ (Sutureless Pterygium Excision with Amniotic Reconstruction and Lamellar Keratectomy) that has resulted in hundreds of ecstatic patients worldwide. Using premium technologies including his own award-winning surgical instruments, Dr. Gulani uses the human placenta (Amniotic Membrane), to not only anatomically correct the area of surgical excision, but also to elegantly and aesthetically cover it giving a dual advantage of a cosmetic outcome along with ocular surface rejuvenation which also addresses the commonly associated dry eyes. He undertakes these intricate microsurgical techniques without stitches (“No-Stitch”) using tissue glue. His proprietary SPARKLE™ technique besides being atraumatic (no injection, no needles) to the patient, and aims for a cosmetic outcome, also prevents recurrence of the pterygium which is the “Achilles’s heel” of traditional pterygium surgeries. Patients from all over the world have been seeking Dr. Gulani’s services and eye surgeons have been flying in to Jacksonville to learn from his techniques and instrumentations.
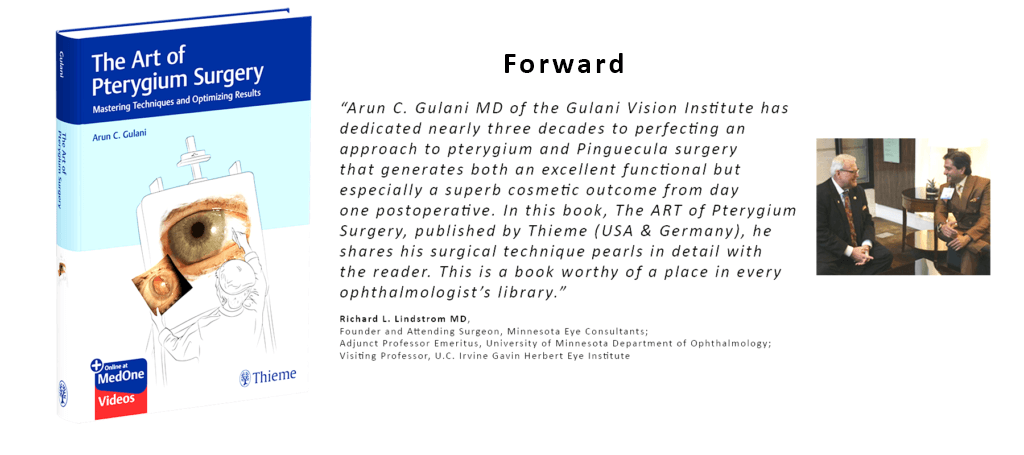
The Art of Pterygium Surgery: Mastering Techniques and Optimizing Results by internationally acclaimed eye surgeon Arun Gulani and esteemed global contributors features an impressive array of collective expertise, pearls, and unbiased approaches. This textbook raises the bar on a challenging surgical procedure in terms of performance, aesthetic outcomes, and patient expectations, while presenting a paradigm shift in defining success beyond lack of recurrence to immediate and long-term appearance of the operated eye.
What started nearly 3 decades ago with celebrities, news anchors, and models seeking our services for cosmetic outcomes of their pterygium surgery has become a common demand of men and women from all walks of life. We see a fair number of professional golfers, surfers, and avid outdoor enthusiasts.
Although prolonged sun exposure is thought to cause pterygium and pinguecula formation, his 30-year experience with patients from the U.S. and worldwide points toward a genetic predilection that was confirmed by observation of bitemporal growths (in both eyes) in children in equatorial countries where we perform pro bono work.
While cosmetic symptoms can seem trivial to ophthalmologists, patient concerns are genuine and range from self-consciousness, low self-esteem, and embarrassment to depression as a result of their ocular appearance. This realization fueled the desire to continuously raise the bar on ocular surface surgery to a cosmetic outcome.
As in LASIK and cataract surgeries in which we aim for spectacle-free vision with a flawless looking eye, we instruct fellows and visiting surgeons that at every step in ocular surface surgery they should constantly think of how they want this patient to look immediately postoperatively and years later. Removing the lesion is one goal and beautifying the eye (with minimal visual impact) is the other goal, but both are essential.
Considering the consistent outcomes of our pterygial surgery, patients have been actively seeking pinguecula correction.
Over three decades, we have classified pterygia into categories (based on head/neck adhesion, vascular pattern, and draw test) and continuously study the presentations and outcomes to improve technique and results. This also underscores the fact that pterygial appearance and size do not predict the surgical ease or outcome.
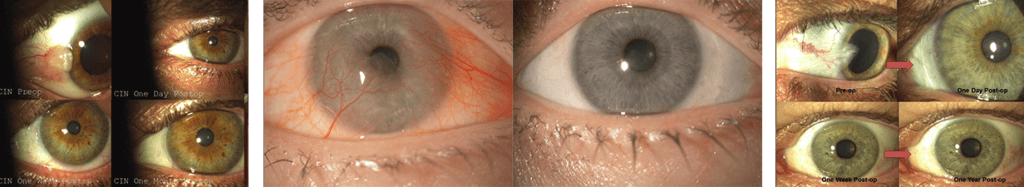
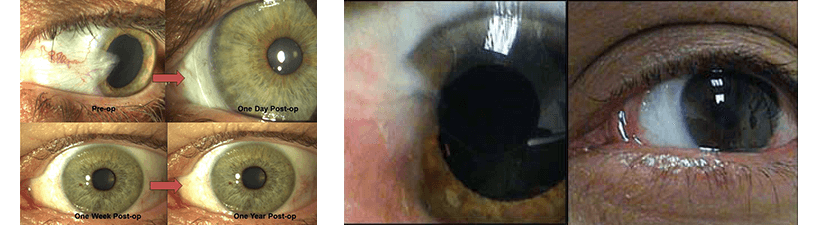
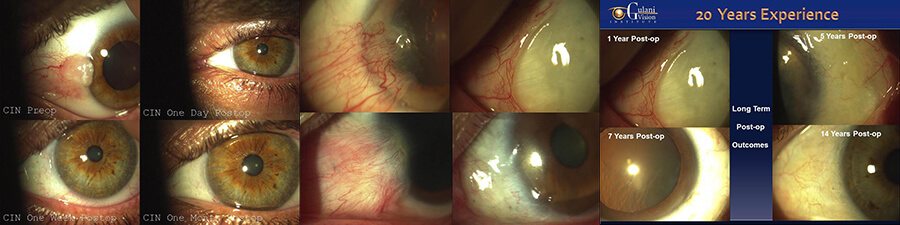
We have honed the “Iceberg Technique” over 3 decades with consistent results. The surgery earned that name because the visible part of the pterygium is just the tip of the iceberg, and the actual growth tends to be much deeper. The surgery enables patients with cosmetic pterygia and pinguecula and those with recurrent and aggressive vision-threatening pterygia to expect clear, white eyes starting day 1 postoperatively.
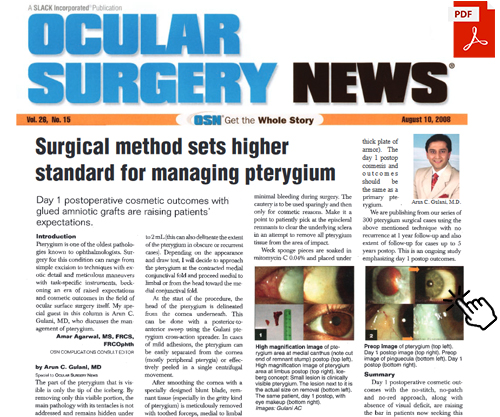
We started out originally with a sutured technique,5 and evolved it to include amniotic grafting with due credit to Dr. Tseng’s work which we incorporated 14 years ago. we then aspired to make it sutureless using the Tisseel Glue (Baxter International) and finally to today’s cosmetic outcomes with refractively neutral endpoints.
Though we have used all kinds of amniotic grafts in the wide spectrum of Cryopreserved and dehydrated varieties, such as Amniograft (BioTissue/TissueTech), Ambiodry (IOP/Katena), and other newer ones on the market including those in research and development internationally, amniotic graft of choice continues to be the Amniograft.
The Iceberg Technique neither threatens nor adversely affects vision because no corneal incisions are made. While the average pterygial recurrence rate hovers near 39%, that with the Iceberg technique has been less than 0.5%.

In a typical case, anesthesia is induced with topical tetracaine hydrochloride (Tetravisc Forte, Sigma Pharmaceuticals) applied preoperatively with topical moxifloxacin (Vigamox, Alcon Pharmaceuticals). Intra-lesional anesthesia (1-2 cc of lidocaine with epinephrine) is used. Recently, patients have been requesting laryngeal mask airway anesthesia. Given that most of these patients are young and healthy and sometimes require extensive surgery, this anesthesia facilitates a comfortable experience and safe recovery.
Depending on the appearance and draw test, we approach the pterygium at the contracted medial conjunctival fold and proceed medially to limbally or from the head toward the medial conjunctival fold.
The head of the pterygium first is delineated under the cornea with a posterior-to-anterior sweep using the Gulani Pterygium Cross-Action Spreader (Storz). In cases with mild adhesions, the pterygium can be separated easily from the cornea (mostly peripheral pterygia and those in elderly patients) or peeled in one centrifugal movement.
After corneal smoothing with a specially designed blunt blade, remnant tissue (especially with gritty pterygia) is meticulously removed with a toothed forceps medially to limbally. The blade is used to smooth the limbus. A wek-cel sponge soaked in 1:1000 epinephrine is tucked into the nasal crevice where the cut pterygium is pressured into hemostasis. When this step is completed, the field is free of blood for dissection. Another benefit is that a space has been created in which to tuck the amniotic graft.
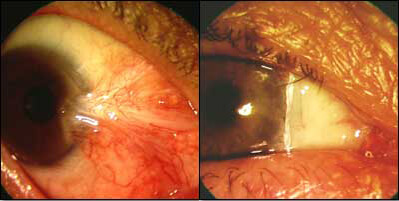
Pterygial dissection is the most important step. The entire pterygial plane is delineated subconjunctivally as if separating a fan-shaped scar with tentacles into the fornices and medial angle. The pterygium is pulled superiorly and vertically to avoid damaging the underlying medial rectus. By cutting vertically instead of horizontally, unnecessary involvement of orbital fat, bleeding, and iatrogenic damage to the medial rectus is avoided.
Upon removal, the pterygium resembles a spreading mass of tentacles. It is important to remove the entire mass to avoid recurrence.
The pterygium is dissected superiorly to avoid buttonholing the conjunctiva and invading the orbital septum and inferiorly to avoid cutting the underlying muscles, which is rechecked after the pterygium is removed.
There is no to minimal intraoperative bleeding. Cautery is performed sparingly and only for cosmetic reasons.
Surgeons should patiently pick at the episcleral remnants to clear the underlying sclera to remove all pterygial tissue from the area of impact. Pieces of wek-cel sponges are soaked in mitomycin C (MMC) 0.04% and placed under the conjunctiva in the area of the dissection for 30 seconds. MMC application on the sclera should be avoided and the sclera dried with a clean wek-cel sponge. After removing all sponges, the area is flushed copiously with balanced salt solution.
The cornea functions as an illuminated receiving table on which to drape the amniotic membrane, which is placed on the raw area and accepted with a Tyre-Tool technique. This eliminates touching the membrane with any instrument, so that it slips under the surrounding cut conjunctival edge medially, superiorly, and inferiorly.
The amniotic graft is milked to adhere to the global contour using a specially designed forceps that squeegees the graft on the sclera. Tisseel Glue is applied under the membrane as two separate components, and the membrane is squeegeed again in two quick sweeps to a pearly white and smooth appearance. The conjunctiva and underlying tenons are glued; they are closed in a C-shape with medial facing convexity to ensure closure of any potential space in between.
The fornices are checked for excessive glue, which can cause irritation and keratitis on the first postoperative day, and cleared with a forceps sweep. The same blade is used in one sweep to cut the excess graft at the limbus. The excess graft is peeled as it clears the cornea and also confirms adhesion of the remaining graft. This ensures that there is no bumpy anatomy at the limbus and patients can resume contact lens wear early postoperatively or undergo laser vision surgery in the near future.
In extensive cases with medial corneal epithelial defects (resulting from peeling of an aggressive pterygium head), we suggest Prokera (BioTissue) or Ambiodisc (Katena) in addition in the postoperative period.
All patients are instructed to look at their eye in a mirror on day 1 postoperatively. We observe their exclamations/reactions, which while always gratifying, vary tremendously based on their cultures and personalities. Most patients are satisfied with their aesthetic results within 24 hours and return to daily activities within a couple of days.
Turning non-candidates into candidates.
The importance of this technique goes beyond successfully treating pterygium and pinguecula and achieving sparkling white eyes 1 day postoperatively. In fact, it is a technique that turns non-candidates who had previously undergone a LASIK or premium IOL cataract surgery with tissue-induced irregular astigmatism, corneal scars, tear film instability, or higher-order aberrations into candidates by removing corneal scars and pterygial tissue with a resultant clear and measurable optical system.
Because many patients have already undergone a LASIK or premium cataract surgery, this technique maintains their optimized vision because LASIK flaps are not distorted, keratitis is not induced, and corneal desiccation/distortion do not occur compared with traumatic techniques or refractively adverse corneal incisions.
We have performed laser vision surgery and implanted multifocal/toric /implantable collamer lenses and even Intacs (Addition Technology) in patients who have undergone the amniotic graft pterygium and pinguecula removal surgery with successful outcomes.
Given the no-cut nature of the grafting procedure, no induced refractive changes occur. Good vision is maintained or even improved by relieving the astigmatism caused by pterygial-induced pull on the cornea.
Despite the consistent results and high patient satisfaction, we place great emphasis on preoperative patient education. Patients are instructed that this is a serious surgical procedure with associated risks. Even with a very low recurrence rate, scarring and worse-looking eyes are possible.
Individual healing patterns play an important role in final outcomes. We suggest caution to surgeons who advertise this procedure under attractive names as We have had numerous patients come to me with complications of these procedures for correction.
One patient who was satisfied with the sparkling white eye postoperatively visited the local eye surgeon who did not see stitches or inflamed red areas postoperatively and tried checking for the graft with a Q-tip across the eye, which removed the glued graft from the eye. The patient returned to me for re-grafting.
The second case was a patient who needed muscle alignment surgery, and the third patient was followed for a localized pupillary shape anomaly that is improving.
All three patients had undergone extensive bitemporal surgery. Although many patients with similar surgical profiles have done very well, we recommend that patients have one lesion removed at a time.
In summary, pterygium and pinguecula surgery can be approached cosmetically, even in extensive cases, and not only improved pathologically and functionally, but also raised to a cosmetic outcome. Additionally, many cases can then benefit from vision correction surgery for associated ammetropia for a concept of “look good and see good!”
This surgery lately has been included in Dr. Gulani’s CORNEOPLASTIQUE™ approach to such eye disorders with a goal for excellent appearance and good vision.
There are various surgical modalities for Pinguecula and Pterygium ie. Eye Bright, I-Brite, Brite Eyes, Amniotic surgery, etc. To find out if you’re a candidate for Dr. Gulani’s world renowned “No-Stitch” surgical technique; SPARKLE™ (Sutureless Pterygium Excision with Amniotic Reconstruction and Lamellar Keratectomy) contact our headquarters in Jacksonville, FL to start your Gulani Vision Experience.